Cognitive Behavioural Therapy
Cognitive Behavioural Therapy (CBT) has the strongest evidence base of all talking therapies for successful treatment of anxiety disorders and depression. It is therefore recommended as treatment of first choice by the UK’s National Institute for Health and Care Excellence (NICE) with a BABCP-accredited expert.
What is CBT?
Cognitive-behavioural therapy (CBT) is all about the relationship between emotions, thoughts and behaviour. It focuses on helping us understand how our thinking about a situation affects the way we feel and act. It’s an active, collaborative and change-focused type of approach, and client and therapist work together to change the client’s behaviours, or their thinking patterns or, most often, both.
CBT is pragmatic and structured, and attending appointments is a starting point. To get the most out of therapy, I ask clients to put things into practice between sessions. Early on in the therapy this might be keeping a diary of thoughts, feeling and behaviours, assigned reading or listening to relevant audio. Later on in the process, we’ll be harnessing our inner scientists, and designing creative challenges that try out new ways of behaving. This might make you feel uncomfortable to begin with, but by repeating these challenges you will get used to behaving differently.
It’s important to me that the hard work you put in during sessions actually leads to changes in your life.
Here’s what to expect
- We will work together to break down your difficulties into separate parts: the situation, thoughts, emotions, physical feelings and actions.
- I might ask you to keep diary or write down your thoughts and behaviour patterns.
- We’ll explore your thoughts, feelings and behaviours to work out if they are unrealistic or unhelpful and to determine the effect they have on you.
- After working out what you can change, we’ll plan how you can practice these changes in your everyday life.
- Confronting fears and anxieties can be challenging so we’ll decide what pace feels comfortable for you. We’ll keep checking back each session on progress and reviewing if we’re moving in the direction you want.
- My aim will be to help you get to the point where you’re confident enough to keep making changes on your own. Sometimes people pop back for a top-up which is fine, but fundamentally, I want to make myself redundant!
How many sessions?
Depending on the issue that brings people to therapy, some see huge improvement in 6-8 sessions when there is a single focus such as sleep disturbance or phobias. More complex or longstanding issues will take a greater number of sessions, so we will have regular reviews along the way to ensure that you are finding CBT helpful.
How problems keep going, according to CBT
Whether you’re experiencing anxiety or more of a depressive problem, we’ll look at the problematic patterns of thinking, feeling and behaviour in a vicious cycle. These cycles highlight the maintaining processes.
Identifying these cycles of unhelpful behaviour is key in the early stage of CBT. We need to be able to recognise patterns, so you can then intercept and change them.
Let’s look at the two most common categories of behavioural maintaining processes: safety behaviours and escape/avoidance.
Safety Behaviours
Safety behaviours occur when you want to protect yourself from something you fear and are often seen in anxiety disorders. For example, if you suffer from panic disorder, examples of this type of behaviour include carrying water ‘just in case’, sitting down if your heart rate increases or taking a diazepam before going on the Tube. Here it is in a vicious cycle:
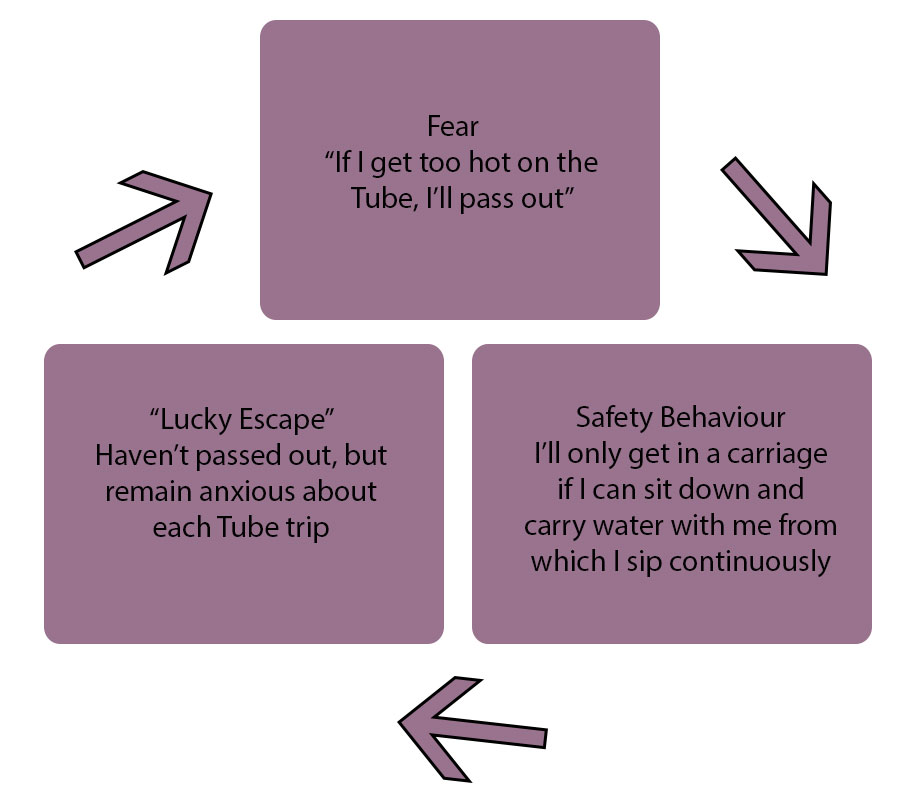
While it’s understandable to try and find strategies that help you cope with unpleasant feelings of anxiety, these behaviours can backfire as the actual problem remains unresolved. This is the case across the disorders, for example, if you’re health anxious, although you managed to feel less anxious the last time you did your daily check for new moles/lumps/changes in your body, you’re going to feel just as anxious tomorrow morning and repeat the behaviour to reduce the unpleasant feelings.
Escape/Avoidance
It’s very common when you’re feeling anxious to want to run away from the situation that is making you feel tense. This is why if you suffer, for example, social anxiety, you might tend to avoid social situations entirely, choosing to be on your own and withdraw. Or you may go, but avoid eye contact, stand on the edge of a group, and hope no one will talk to you. Like other safety behaviours, avoidance and escape can actually make your anxiety worse in the long run, because they undermine your confidence and prevent you from discovering if your fears are founded on reality, or are just extreme and unhelpful
Become your own therapist
Unlike more traditional forms of therapy, CBT (and I) firmly believe that you have the power to break out of this cycle, and my role is to help you discover how, either face to face or online.